If you’re working in general practice, performing a blood transfusion or administering plasma could potentially only be a once-in-a-blue-moon occurence, but here at Animal Emergency Australia, our critical patients often require transfusions on a regular basis. Sometimes every single shift! And for veterinary professionals who haven’t already encountered transfusion medicine, it can potentially be a daunting process if you’re unfamiliar. That’s why we’ve put together this handy guide to canine and feline transfusion medicine to hopefully take some of the confusion out of your next transfusion.
The most basic question we get asked about transfusion medicine and the most important to answer is – “When should I give blood?” This is then followed closely by several equally important questions: “What type of blood do I give? How much to give? And how fast to give it?” These are just a few of the questions we aim to answer for you in our AEA Guide to Transfusion Medicine.
What Type of Transfusion?
The type of transfusion given should always be based on the individual needs of the patient. And admittedly, when discussing transfusion medicine, many veterinary professionals are likely to think of blood transfusions. But transfusion medicine can be about far more than just blood! In fact, transfusion can refer to any of these 5 different types of blood products:
- Whole blood
- Packed Red Blood Cells (pRBCs)
- Fresh Frozen Plasma (FFP)
- Frozen plasma (FP)
- Other transfusions – given more often in a referral hospital under specialist supervision
- i.e., albumin, lyophilized platelets
But how do you know which of these to use and when?
Whole Blood – If you need to address acute haemorrhage, where there is a concurrent loss of coagulation factors, RBCs and blood volume, then the best choice may be fresh whole blood to replace exactly what has been lost.
Packed Red Blood Cells – If dealing with a chronically anemic patient, where they are often euvolaemic, then your goal is to raise the PCV to deliver more oxygen to the tissues without volume overloading them, meaning the best choice would be pRBCs.
Plasma – Finally, if we are addressing a coagulation disorder due to lack of coagulation factors or possibly toxicity (snake bite, Vitamin K antagonists etc.), then fresh frozen or frozen plasma would be the transfusion most fitting for our situation.
There are times, however, that the type of transfusion will be limited to what is available in your clinical setting and which readily-available transfusion will be the most useful for your patient. In these circumstances, consider which you have access to, and will be most appropriate in each case.

Fresh Frozen Plasma (FFP) vs. Frozen Plasma (FFP)
Yep, even with such similar names, they’re two different products! Fresh frozen plasma (FFP) is made from a fresh, anticoagulated, whole blood donation that has been separated into two parts: the packed red cell portion and plasma by centrifugation. In order for it to be called FFP, this process needs to have occurred within 8 hours of the donation being made. FFP contains labile clotting factors (fibrinogen, FV, FVIII, vonWillebrand’s factor) as well as non-labile factors (FII, FVII, FIX, FX, FXI), immunoglobulins, albumin, lipids and electrolytes. It DOES NOT contain viable platelets.
Frozen plasma (FP) is the anticoagulated portion of centrifuged blood if the separation has occurred later than 8 hours from collection or FFP that has been stored past its expiry date. It contains the non-labile clotting factors (FII, FVII, FIX, FX, FXI) but will have variable amounts of labile clotting factors, immunoglobulins, albumin, lipids and electrolytes.
When Should I Transfuse?
When deciding whether or not to give a transfusion, we need to remember that transfusion medicine is not an exact science. Each time we are faced with the possible need for a transfusion, we should take it on a case-by-case basis with thorough clinical assessment of the patient and basic supportive bloodwork.
The best way to break it down is to recall the main function of the blood itself; the transport of oxygen and nutrients, the formation of clots to prevent blood loss and the transport of immune cells to help fight infection. Knowing this, we can then form some general guidelines that can help us in our decision-making process. The clinical signs indicating a transfusion of whole blood or packed red blood cells is needed are known as “transfusion triggers“.
When to Transfuse Whole Blood or Packed Red Blood Cells
These are the main transfusion triggers in which patients will benefit from a transfusion of either whole blood or packed RBCs:
- A peracute decrease of PCV below 25% (dogs) and 20% (cats)
- PCV below 15% (likely to be impacting the delivery of oxygen to the tissues (DO2))
- If going to surgery and PCV is below 20% in a dog and 18% in a cat
- Decreased SPO2
- Prolonged Tachycardia (keep in mind a HR taken after a gentle walk will give much more information in an anaemic animal, as usually they have learned to cope with anaemia at rest but when light exercise is introduced it unmasks the inadequate DO2)
- Hypotension (post blood loss)
- Increased lactate and base deficit (indicating inadequate DO2 and conversion to anaerobic metabolism)
- Poor pulse quality
- Marked blood loss during surgery as anaesthesia decreases cardiac output and therefore will decrease DO2 further in an already anaemic animal
Each of these transfusion triggers should also be considered based on the individual patient.
When to Transfuse Plasma
There are also several situations where plasma will be the more ideal choice for your patient, especially when taking advantage of the more concentrated clotting factors in comparison to whole blood. These include active bleeding with:
- Anticoagulant toxicity (rodenticide, snake bite, xylitol)
- Angiostrongylus infection
- Von Willebrands disease or haemophilia
- DIC
- Post surgical consumptive coagulopathy
- Liver biopsy

How Much to Transfuse and How Fast
It’s important to keep in mind when deciding how much blood to give that a PCV over 30% will cause increased viscosity and actually decrease CO, so consider choosing a PCV goal below this. Also, when considering how much blood to give, remember there is no maximum dose of blood or plasma. Blood products are given to effect and therefore need constant monitoring is required, which we’ll discuss in further detail below. The following are starting doses (usually rounded to the nearest half or whole unit of blood product once calculated):
- Whole blood – 20-25ml/kg
- pRBC’s – 10-15ml/kg
- Fresh frozen plasma – 10-15ml/kg
Transfusion Dosage Calculations
Dogs: Volume to give = BWT (kg) x 85 x [(goal PCV – Recipient PCV) / Donor PCV]
Cats: Volume to give = BWT (kg) x 65 x [(goal PCV – Recipient PCV) / Donor PCV]
Given the constraints with blood collection in cats, we usually only have access to 50-60mL of freshly collected whole blood. In some cases, larger referral hospitals may have access to donor cats where they can collect and store blood as required.
How to Administer a Transfusion
All frozen products need to be brought to room temperature before administration by immersion in a warm water bath. Thawed units should be used within 24hrs and should not stay at room temperature for longer than 4 hours. Blood products need to be administered through a dedicated IV catheter where possible as other medications/fluids administered concurrently can cause derangements in coagulation. All blood products should be administered via a syringe pump
or volumetric pump validated for blood components with the use of an administration set with incorporated filter.
Transfusion Rates
The initial rate for the transfusion is slow in order to monitor for reactions. If a reaction is to occur, the signs are likely to manifest in the initial stages of the transfusion. There are many different protocols available for starting a transfusion, but they all begin with a slow initial rate. Most commence at a rate of 0.25–1 mL/kg/hr, or 25–50% of the calculated target rate for the first 15–30 minutes. The patient is closely monitored during this time and the vital parameters are obtained every 5 minutes. If any changes to the parameters occur, the transfusion is halted and the veterinarian in charge notified for immediate examination.
Some protocols may include an intermediate rate which calls for an increase of 50–75% of the target rate, which is then monitored closely for another 15–30 minutes.
Once our initial (and intermediate if using this) rates have been administered without any sign of a reaction, the remainder of the transfusion can be given within the allotted 4 hours. The patient should continue to be monitored every 15-30 minutes for the entire course of the transfusion. In an emergency situation we may need to give blood rapidly as an IV bolus, usually this is over 10-15 minutes. Faster administration will increase the chances of a transfusion reaction, but in a life or death situation this is a risk we have to take.
Monitoring During Transfusions
Vigilant monitoring during transfusion medicine is essential, as any kind of transfusion has a chance to cause reactions. A nurse/technician should be dedicated to monitoring the transfusion for the earliest detection of any possible complications. The patient needs to be monitored throughout the transfusion and vitals should be recorded on a transfusion monitoring sheet that is kept as a part of the patient’s medical record.
A baseline set of vitals should be obtained before the transfusion begins so that they can be referenced and compared to during the transfusion. This includes heart rate, respiratory rate and effort, pulse rate and quality, mucous membrane colour, capillary refill time, mentation/attitude, temperature, and blood pressure. Other known symptoms such as vomiting and diarrhoea prior to the transfusion should also be noted. During the transfusion the same parameters are monitored intermittently and any small changes noted and responded to. Other signs such as facial swelling, urticaria, pruritis, are monitored as well.
Monitoring of reactions should be continued after any transfusion for at least 24 – 48hrs. A red blood cell level should be assessed immediately post transfusion and then again 8 – 24hrs later. Evaluation of the patients plasma and urine output is recommended to monitor for delayed haemolytic reactions. The patient should also be closely monitored for any changes in respiration.
Transfusion Reactions
Below is a quick reference chart outlining several common forms of reactions to transfusion therapy, which we’ll also explain in further detail.
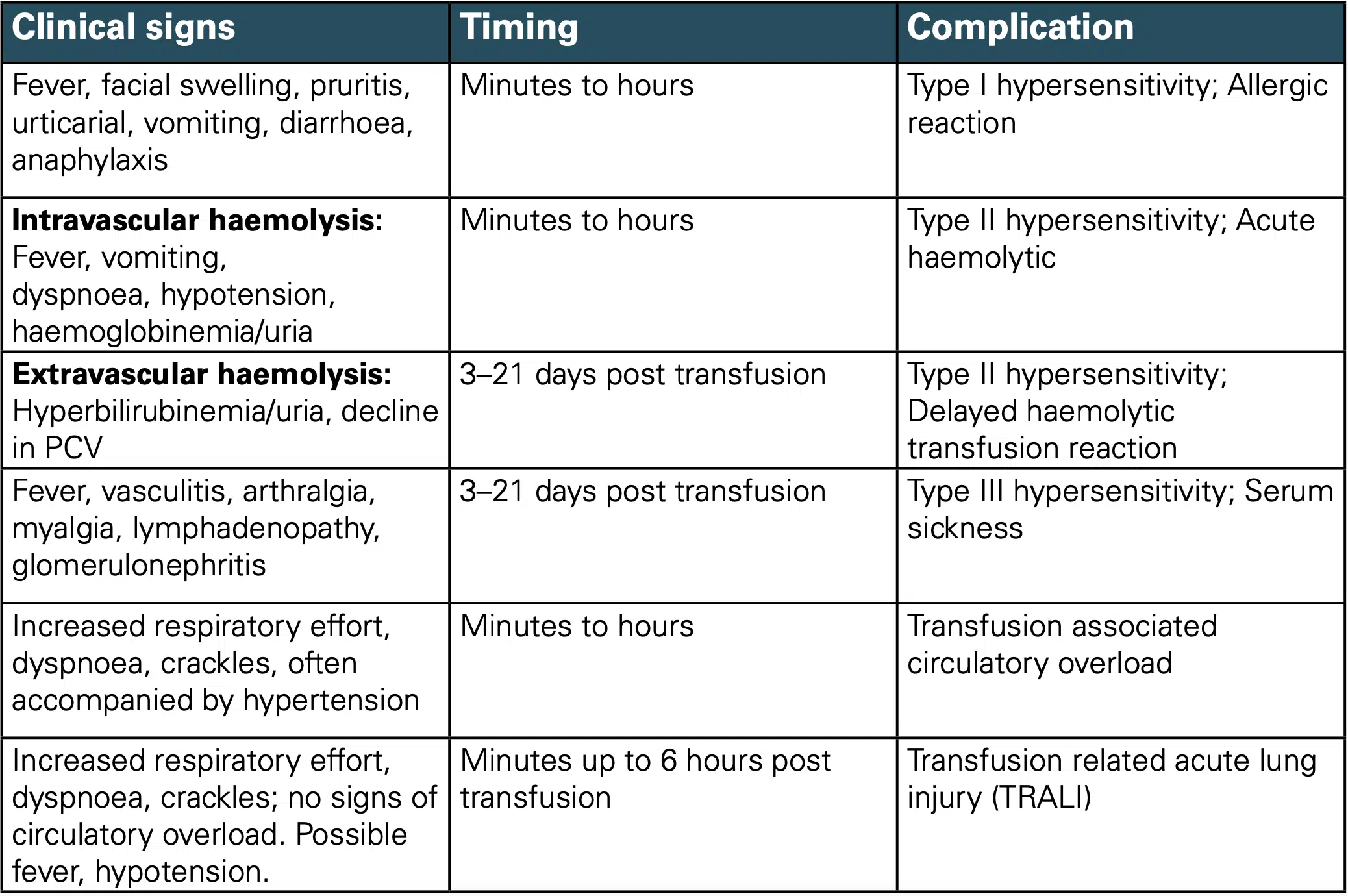
Immunologic Transfusion Medicine Reactions
Allergic Reactions
Pathophysiology: Type 1 hypersensitivity reactions to an antigen within the blood product. This is mediated by IgE and leads to mast cell degranulation as well as production and release of various inflammatory mediators (e.g. histamine, prostaglandins, leukotrienes). These can range from mild and self-limiting through to life-threatening anaphylaxis.
Time frame: Typically occur within 4 hours of transfusion (most commonly within 1 hour of transfusion initiation).
Clinical signs: Most common type of reaction, typically mild respiratory, cutaneous and/or GI signs.
Treatment:
- Mild reactions: Antihistamine (e.g. chlorpheniramine 0.5mg/kg IM q8hrs)
- Anaphylaxis: STOP TRANSFUSION and administer adrenaline 0.1-0.5mg/cat or up to 2 boluses of 0.1-0.2mg/kg IM followed by 0.05- 0.1ug/kg/min IV)
- IV crystalloid fluid boluses should be given to patients in shock
Immunological Haemolytic Transfusion Reactions
Acute Haemolytic Transfusion Reactions (AHTR)
Pathophysiology: Type II hypersensitivity to major or minor incompatibilities between donor and recipient erythrocytes. Occurs from destruction of donor or recipient erythrocytes and is caused by blood type incompatibilities.
Clinical signs: Characterised by acute haemolysis.
Time frame: Within first 24 hours of blood transfusion.
Treatment:
- STOP TRANSFUSION AND DO NOT RESTART!
- Monitor airway, breathing and circulation
- Supportive therapy: IVF, oxygen and vasopressors for hypotension
Delayed Haemolytic Transfusion Reaction
Pathophysiology: Immune response to donor erythrocytes such as xenotransfusion of canine to feline patients; AB-mismatched feline allogenic transfusion (type B to type A cats).
Time frame: 24hrs to 28 days after transfusion
Febrile Non-Haemolytic Transfusion Reactions
Pathophysiology: Immunologic or non-immunologic such as donor leukocyte or platelet antigen-antibody reactions or transfer of proinflammatory mediators within stored blood products. More common when given blood with long storage time. In cats, a mismatched transfusion is the most common cause.
Clinical signs: Temperature of > 39 Celsius degrees with > 1 degrees Celsius increase from pre-transfusion body temperature.
Time frame: Within 4 hours of transfusion
Treatment: Typically self-limiting and does not require therapy with antipyretics. Currently there is insufficient evidence as to whether slowing transfusion rates is helpful or not.
Transfusion-Related Acute Lung Injury (TRALI)
Pathophysiology: Acute, immunologic reaction to antigen-antibody interactions within the lungs which is rare in dogs and does not appear in cats. Currently the cause is unknown but suspected that transfused cytokines induce neutrophils to adhere to pulmonary endothelium, releasing proteases and causing endothelial damage.
Time frame: Acute to within 6 hours of initiation of transfusion.
Clinical signs: Acute hypoxaemia and non-cardiogenic pulmonary oedema
Post-Transfusion Purpura
Pathophysiology: Delayed immunologic reaction caused by alloimmunisation against platelet antigens only caused by transfusion of any platelet-containing blood product. Very rare in dogs and not seen in cats.

Non-Immunologic Transfusion Medicine Reactions
Transfusion-Associated Circulatory Overload (TACO)
Pathophysiology: Volume overload.
Time: Within 6 hours of transfusion.
Clinical signs: Acute respiratory distress and hydrostatic pulmonary oedema.
Risk factors: Rapid transfusion, underlying cardiac disease, renal failure, or normovolaemic anaemia.
Treatment:
- Diuretics (e.g. furosemide 1-2mg/kg IV initially)
- Oxygen therapy PRN
- If pleural effusion develops, consider thoracocentesis
Transfusion-Associated Dyspnoea
Pathophysiology: Any respiratory associated transfusion reactions that does not fit well within TRALI or TACO categories.
Clinical signs: Acute respiratory distress during or within 24 hours of transfusion.
Differential Diagnoses: TACO, TRALI, allergic reaction, or unrelated pulmonary disease.
Non-Immunologic Haemolytic Transfusion Reactions
Pathophysiology: thermal mechanical, osmotic or chemical factors that damage transfused erythrocytes.
Transfusion-Transmitted Infections (TTI)
Pathophysiology: Contamination during collection, storage or administration. Bacteria are more likely to proliferate in stored erythrocyte products or fresh platelet products. Can include bacteria such as E.coli, Pseudomonas, Serratia, Enterococcus, Staphylococcus spp., Bacillus, Cornebacterium, or blood-borne organisms including Mycoplasma spp., Anaplasma, FeLV, FIV, Babesia spp., Cytauxzoon spp., Leishmania spp., Bartonella henselae, and Rickettsial agents.
Clinical signs: Pyrexia secondary to sepsis typically more severe than FNHTR.
Treatment: Broad spectrum IV antibiotics whilst awaiting blood culture results.
Citrate Toxicity
Pathophysiology: Caused by the anticoagulant that chelates calcium, which can lead to significant hypocalcaemia within hours of transfusion.
Risk factors: Large volumes of blood products infused rapidly or transfusions given to patients with severe liver disease.
Time frame: Acute
Treatment: Calcium supplementation (5-15mg/kg elemental calcium slow IV over 20-30 mins or 2.5-3.5mg/kg/hr IV) for patients requiring large volume transfusion. NB: do not administer calcium through the same line as transfusion IV line.
Hyperammonaemia
Pathophysiology: Acute reaction that occurs in patients with severe hepatic dysfunction or failure. This is due to the fact that ammonia levels increase in stored blood products over time. Unlikely from single transfusion unless underlying hepatopathy are present or are premature neonates with decreased liver function
iv. Very rare in dogs and no cases reported so far in cats.
Hypothermia
Pathophsyiology: Small patients receiving large volumes of products that have not been warmed sufficiently.
Treatment: Correct hypothermia.
Hypotensive Transfusion Reactions
Pathophysiology: Activation of coagulation factor XII increases bradykinin, leading to vasodilation and increased vascular permeability. Associated with administration of ACE inhibitors before or during a transfusion. Can also be due to use of post-storage, leuko-reduced blood products. Rare in dogs and not been reported in cats.
Time frame: Acute.
Clinical signs: Significant hypotension.
Treatment: Correct hypotension.

Final Points to Consider About Transfusions
- Blood is not a cure all and should not be used prophylactically without correcting the underlying cause of anaemia.
- There is no proof that plasma improves the outcome of pancreatitis in patients unless they are coagulopathic or hypoalbuminaemic.
- There is no evidence that premedication will reduce transfusion reactions.
- Typed and cross-matched transfusions decrease reactions.
- The use of leukoreduction devices has been shown to reduce transfusion reactions, so should be used where available.
- Steroids have not been found to have any effect on transfusion reactions and in fact, and may even be detrimental. For example, a single dose of dexamethasone in a hypoxaemic or hypovolaemic dog can cause GIT ulceration.
- Blood transfusions should be finished in 4 hours once spiked to minimise bacterial growth in the blood product.
- Strict asepsis is vital to avoid bacterial contamination.
- Do not administer blood with calcium containing fluids (e.g. Hartmann’s/Lactated Ringer’s solution), hypotonic or hypertonic solutions.
- Fluid overload in cats (especially when using whole blood volumes) is a very real concern.
We hope this guide to transfusion medicine helps you approach your next transfusion with confidence and helped answer some of your questions around transfusion medicine! You can also sign up to VetAPedia to download the full protocol as a handy PDF to keep in your clinic to reference at any time. And be sure to visit more of our patient care resources at AEA where we’ll have more on transfusion medicine with an upcoming guide to blood-typing and cross-matching.